50 /m cellulitis with AKI on ? CKD with heart failure with reduced EF ,CAD - S/P PTCA
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
50 year old male daily wage labourer presented to the casualty with the complains of
Right lower limb ulcers and swelling since 1 month
shortness of breath since 10 days
HISTORY OF PRESENT ILLNESS
patient was apparently asymptomatic 1 month ago he then had an thorn prick injury to his right leg , following the injury 2nd day patient had mild redness and swelling over that region, the swelling progressed gradually and started developing ulcers over that region, there was blacking discoloration over that region and gradual pus discharge from that site , the wound gradually extended to the right foot and leg .
History of fever following swelling of the right lower limb , high grade , associated with chills and rigors intermittent , no diurnal variation and relieved after medication, fever subsided after 5 days.
Patient was taken to near by hospital and was diagnosed to have right lower limb cellulitis with acute kidney injury (AKI )
where debridement was done and left femoral catheter was placed , during the hospital stay patient received 7 sessions of haemodialysis
Patient started experiencing shortness of breath since 10 days insidious in onset and gradually progressive progressed from grade II to IV associated with orthopnea and no PND
No diurnal variation and no seasonal variation of shortness of breath
No history of cough , chest pain , pedal edema, vomitings, giddiness, palpitations
Routine 2d echo done there showed RWMA and EF of 35% and patient was referred to our hospital for further evaluation and management
Time line of events
Patient is the 4 th born member of the family 3 elder sisters and 2 younger sisters and brothers
Patient is illiterate and helped their parents in farming
Got married at the age of 19 years to 15 year old women and non consanguinous type of marriage
Had 2 childern one male and female
Patient daily routine is to get up at 5 am go to farm for milking the cows and feeding them , comes back home at 7 am, has breakfast at 9 am and goes to daily wage labourer work - where he used to carry mud and other agricultural goods and goes for ploughing comes back home at 6 pm then goes out with his friends for recreational activity consumed daily 2 quarters of alcohol and 12-16 beedis for day and goes to bed at 9 pm after having dinner
Patient was doing well till the last 10 years
10 years ago his son who was normal and healthy all of the sudden was found dead at home by the evening they came home from the work
From then patient was more addicted to alcohol and smoking and never used to have proper food and used to feel saying that my son was dead
His daughter got married 6 years ago
From then the patient and his wife were living together and doing their daily work and patient continued to drink alcohol in increasing quantity and consumed 20 beedi per day
2 years ago in the month of February patient had sudden onset chest pain, giddiness and shortness of breath and was diagnosed to have acute MI and angiogram was done PTCA was done patient was discharged with rosuvastatin20 mg + ecosprin 75 mg + clopidogrel 75 mg , carvedilol 3.125 mg.
Patient was using regular medication for his heart problem since then
Six months later he was diagnosed to have hypertension and was started on medication
2 months later he was diagnosed with hypothyroidism and was started on thyronorm 25mcg
Patient was using all these medications and was doing well and since his heart surgery he was restricted to home and did not go for workk
1 month ago he developed thorn prick injury and eventually AKI and heart failure and 7 sessions of HD and wound debridement was done and was referred to our hospital
Past history
H/O CAD - S/P PTCA 2 yrs ago on TAB. ECOSPRIN 75 MG + TAB. CLOPIDOGREL 75 MG + ROSUVASTATIN 20 , TAB. CARVEDILOL 3.125 MG PO/OD, TAB.
K/C/O HYPERTENSION since 6 months
Family history
No significant family history
PERSONAL HISTORY:
Appetite-Decreased
Diet - Mixed
Bowel - decreased urine output since 1 week
Bladder -Regular
Sleep - Decreased.
General examination:
Patient is conscious, coherent, cooperative, well oriented to time , place and person
Pallor - present
Icterus - absent
Cyanosis - absent
Clubbing - absent
Lymphadenopathy- absent
Pedal edema - absent
VITALS : Temp - 99.6 F
PR - 118 bpm, regular
BP - 100/60 mmhg
RR - 26 cpm
SPO2 - 96% onRA
GRBS - 102 mg/dl
Systemic examination
CVS -
INSPECTION
Shape of chest is elliptical.
Raised JVP present
Apex best in 5 th and 6 th intercostal space in mid clavicular line
No visible pulsations, scars , sinuses , engorged veins.
Trachea is central
Palpitation:
No local rise of temperature and no tenderness
Apex beat - felt at left 5th intercostal space
No palpable heart sounds
No thrills and parasternal heaves
Auscultation :
S1 and S2 heard.
PER ABDOMEN:
Inspection :
Umbilicus is central and inverted
All quadrants are moving equally with respiration
No scars , sinuses , engorged veins, visible pulsations .
Hernial orifices are free.
Palpitation :
Abdomen is soft and non tender .
No organomegaly.
Percussion :
Tympanic note heard over the abdomen.
Auscultation:
Bowel sounds are heard.
RESPIRATORY SYSTEM:
Inspection:
Shape- elliptical
B/L symmetrical ,
Decreased movements on right side mammary region, infra scapular region .
Engorged veins on the left side
No scars, sinuses, pulsations
Palpation:
Inspectory findings are confirmed
Trachea - central
AP diameter 16 cm
Transverse diameter 23 cm
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion:
Dull note on right mammary, interscapular infra axillary, infrascapular
Auscultation:
bilateral air entry present. Normal vesicular breath sounds heard. Decreased breath sounds on right mammary, interscapular infra axillary, infrascapular
CENTRAL NERVOUS SYSTEM:on the day of presentation
Conscious,coherent and cooperative
Speech- normal
No signs of meningeal irritation.
Cranial nerves- intact
Sensory system- normal
Motor system:
Tone- normal
Power- bilaterally 5/5
Reflexes Right Left
Biceps ++ ++
Triceps ++ ++
Supinator ++ ++
Knee ++ ++
Ankle ++ ++
At presentation
After regular dressings
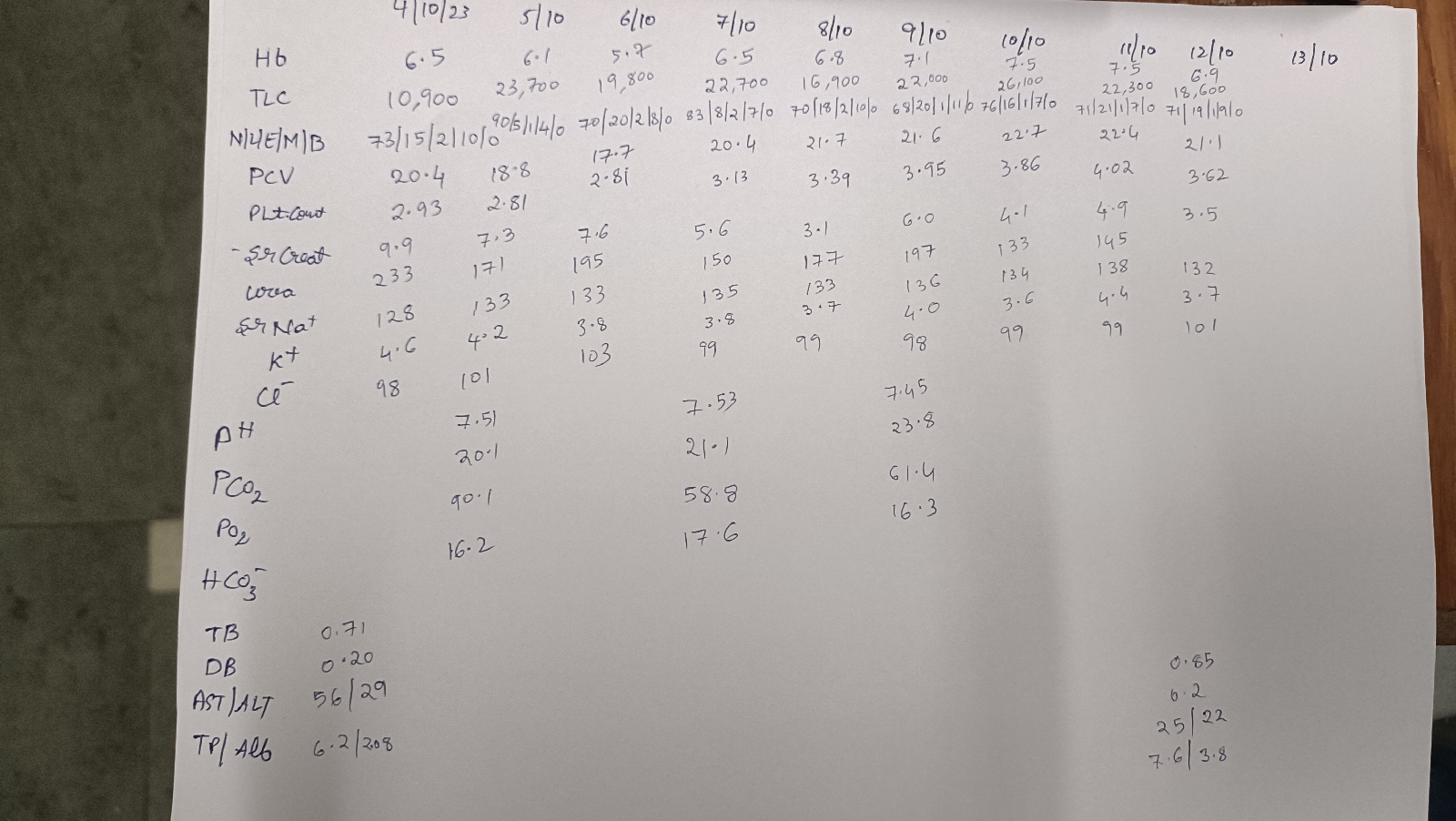
Serial lab investigations