60/F with CAD- heart failure with reduced ejection fraction on mechanical ventilator , severe lv dysfunction left upper lobe fungal ball aspergilloma , VT - SR, diabetic ketoacidosis, diabetic foot ulcer
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centred online learning portfolio and your valuable inputs on the comment box is welcome."I've been given this case to solve in an attempt to understand the topic of "patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan
CHIEF COMPLAINS
60 year old female daily wage labourer by occupation, resident of Tirumalagiri, mothkur presented to the casualty on dec 25 th 2023 with the complains of pedal edema since 5 days, shortness of breath since 3 days
BACKGROUND HISTORY
Born in a rural village, parents were daily wage labourers,
6 th member of the family, among 7 siblings, 3 brothers and 4 sisters
|
Uneducated, helped their parents in household things and at farm
|
Married at the age 14 yrs to a daily wage labourer
|
Had 3 children - 2 sons and 1 daughter by the age of 20 yr
|
Got all the children married and leading an uneventful life till 15 yrs ago
|
Daily routine : wake-up at 4:30 am in the morning the couple together goes to farm for milking the cows and feed them
Get back to home at 7 am in the morning
Cook their breakfast ( jowar roti, ragi Jawa , chapattis, Upma )
Goes to their daily wage work from 9 am and come back to home by 6 pm, their work consisted of harvesting rice fields , groundnut fields , cotton fields
Gets their dinner by 8 pm and goes to bed by 8:30 pm
|
15 yrs ago suddenly her elder son while driving tractor had accident and expired
The couple was distressed a little as they had to look after their sons kids
|
Later his elder son wife left the home and stayed with their parents
|
12 yrs ago patient had fever, burning micturition with generalised weaknesss and was diagnosed as diagnosed as type II Diabetes mellitus and was taking Glimiperide 1 mg+ Metformin 500mg tablet once daily
|
Later due to their old age they could not go to their daily wage works and started staying at home
They started depending on their younger son for their food
|
Their younger son was not taking care of them properly
|
They used to spend half of their month with son and half month with daughter
|
Her husband had CVA 3 yrs ago on waking up from sleep and had right hemiparesis after which he recovered gradually after 6 months
|
Patient had family stressors in the form of property disputes between both the daughter in laws, they were not looked after and they did not have food and money for medications
|
About 50 days ago Patient had vomitings daily 4 to 5 times watery in consistency, non projectile, non bilious, non blood stained, this continued for 4 to 5 days, and generalised weakness for which her daughter took her to local RMP and he gave iv fluids.
Then he noticed some swelling in the in the left foot up to and small ulcer on the base of the 3 rd toe on plantar aspect
He advised them to go for to a general surgeon for that wound management
|
Patient also developed blackish discolouration of the 3rd toe of left foot, the patient observed it 2 to 3 days after the symptoms started. Patient was then taken to a general surgeon where they diagnosed her to have diabetic ulcer with gangrene and adviced amputation of the 3 rd toe and ulcer debridement
Due to financial issues patient could not get it done there, and came to our hospital for further management
|
Patient got admitted in our hospital on 13-12-2023 for diabetic wound management in general surgery department
During the hospital stay patient was found to have decreased breath sounds, b/l basal crepts and Pulmonology opinion was taken and diagnosed to have left upper lobe fungal ball and b/l pleural effusions
Bronchoscope was adviced for further evaluation and management but patient attenders were not willing and did not give consent for the procedure
On 21 st December after the wound was found to be in healing stage patient was discharged from the hospital
|
Patient was doing well in the home for 2 days
Later she gradually started developing shortness of breath
HISTORY OF PRESENT ILLNESS
66 yr old female presented with complains of pedal edema for both legs since 5 days and shortness of breath since 3 days
Pedal edema was insidious in onset , pitting type extending up to the knee joint , not associated with pain.
Shortness of breath since 3 days insidious in onset and gradually progressive, progressed from grade II to grade IV , associated with Orthopnea, no PND, no aggravating and relieving factors, no diurnal variations.
Decreased urine output since 3 days
Ulcer over the left foot on both plantar and dorsal aspect extending from the base of 3rd metatarsal to dorsum of the left foot
No H/o chest pain, palpitations, pedal edema, vomitings giddiness, loose stools, Excessive sweating.
PAST HISTORY
History of diabetes since 12 years using human actrapid insulin since 1 week (previously metformin 500mg and glimiperide Per oral once in the morning)
Not a known case of hypertension, epilepsy, CAD, CVA, thyroid disorders, epilepsy
H/o disarticulation and debridement of 3rd toe of left foot 12 days back
FAMILY HISTORY
No significant family history
PERSONAL HISTORY
Appetite decreased
Bowel and bladder movements normal
Mixed diet
Drinks toddy occasionally once a month
GENERAL EXAMINATION
Patient is drowsy , but arousable
GCS- E 3 V 2 M5
Moderately built and nourished
Pallor present
Pedal edema pitting type extending up to the knee joint
No icterus, lymphadenopathy, clubbing, cyanosis
VITALS
PR: - 140 beats per minute
Temperature: - 98 F
Respiration: - 32cpm
Blood pressure: - 90/70 mmHg
GRBS: - 419mg/dl
SYSTEMIC EXAMINATION :
CARDIOVASCULAR SYSTEM
INSPECTION :
•Elliptical and Bilaterally symmetrical chest
• Apical impulse at left 5 th ICS
• Trachea appears to be central in position
JVP is elevated
•No visible pulsations/engorged veins/scars/sinuses on chest wall.
PALPATION
Apex beat diffuse - palpable at left 5th and 6 th Intercostal space at midclavicular line.
Right Parasternal heave present
No thrills present
AUSCULTATION
S1 and S2 normally heard.
Pan systolic murmur heard at left 5 th ICS
RESPIRATORY SYSTEM
INSPECTION:
Chest bilaterally symmetrical
Trachea is central in position
Chest movements are symmetrical on both sides
Intercostal muscles retractions seen
No scars.
No visible pulsations Apical impulse not seen
PALAPTION:
No local rise of temperature
No Tenderness
All inspectory findings are confirmed
Trachea is central ,chest movements are symmetrical on both sides
Tactile Vocal Fremitus: Normal in all areas
PERCUSSION :
Resonant note heard in all areas.
AUSCULTATION :
Bilateral air entry present
Normal Vesicular Breath sounds heard
B/L diffuse crepts present
PER ABDOMEN
Shape of abdomen - scaphoid
No visible pulsations/engorged veins/scars/sinuses.
Soft, Non tender.
No guarding and rigidity.
No organomegaly
No suprapubic bulge.
Bowel sounds present.
CENTRAL NERVOUS SYSTEM :
Higher mental functions :cannot be elicited.
Bilateral Pupils: Normal in Size and reacting to light.
Cranial Nerves: cannot be elicited
Sensory system – cannot be elicited
Motor System : Power Right Left
Upperlimb 5/5 5/5
Lowerlimb 5/5 5/5
Tone – Normal in all 4 limbs
Reflexes – Biceps Triceps Supinator Knee Ankle
Right ++ ++ + ++ +
Left ++ ++ + ++ +
Plantor - Flexion in both limbs
Cerebellar examination - cannot be elicited
Gait - cannot be elicited
Spine and skull -Normal
LOCAL EXAMINATION
———-
————-
——————
On subsequent dressings
INVESTIGATIONS :
Haemogram :
HB : 8.2 gm/dl
TLC :25,000/Cummins
N/L/E/M/B : 86/6/0/6/0
PCV :25.4
PLATELET: 7.6 lacs/Cummins
COMPLETE URINE EXAMINATION :
ALB : nil
SUGARS: trace
PUS CELLS : 3 to 4/Hpf
EPITHELIAL CELLS : 2 to 3 /hpf
URINE FOR KETONE BODIES - positive
SEROLOGY
HIV I & II - negative
HCV - negative
HBsAG - negative
RENAL FUNCTION TESTS
BLOOD UREA- 27 mg/dl
SERUM CREATININE - 1.1 mg/dl
SERUM CALCIUM - 10.0 mg/dl
SERUM SODIUM - 135meq/l
SERUM POTASSIUM - 4.8meq/l
SERUM CHLORIDE - 105meq/l
LIVER FUNCTION TESTS
TOTAL BILIRUBIN- 0.97mg/dl
DIRECT BILIRUBIN - 0.19mg/dl
AST 47 IU/L
ALT 14 IU/L
ALP 190 IU/L
TOTAL PROTEINS 6.0 gm/dl
ALBUMIN 2.85gm/dl
A/G ratio 0.90
PT 19 sec
INR 1.4
APTT 39 sec
ABG
PH -6.95
PCO2- 62mmhg
PO2-88mmhg
So2-85
HCO3 13mmol/l
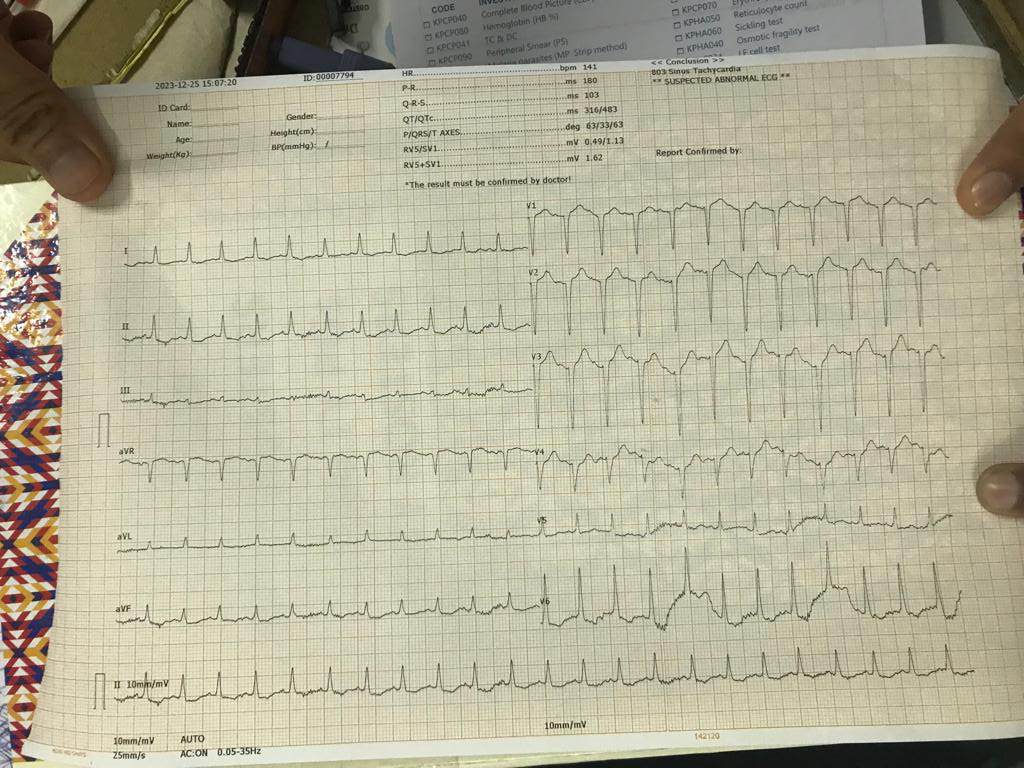
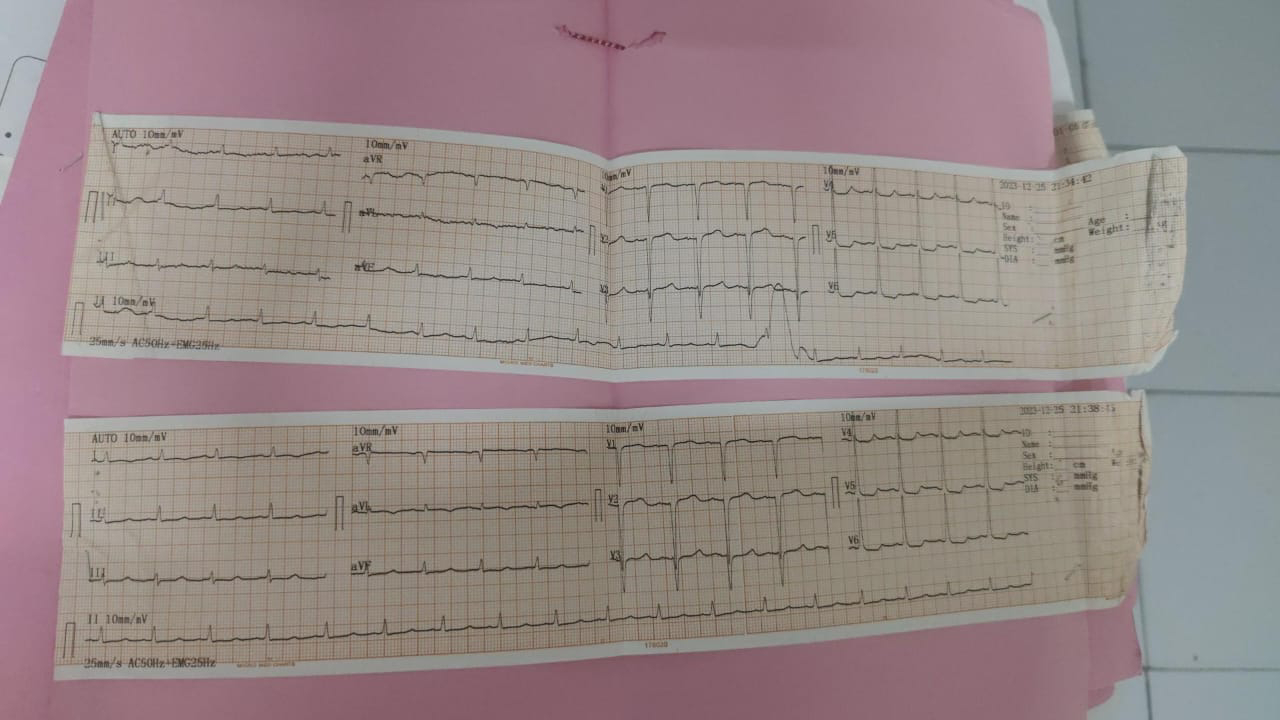
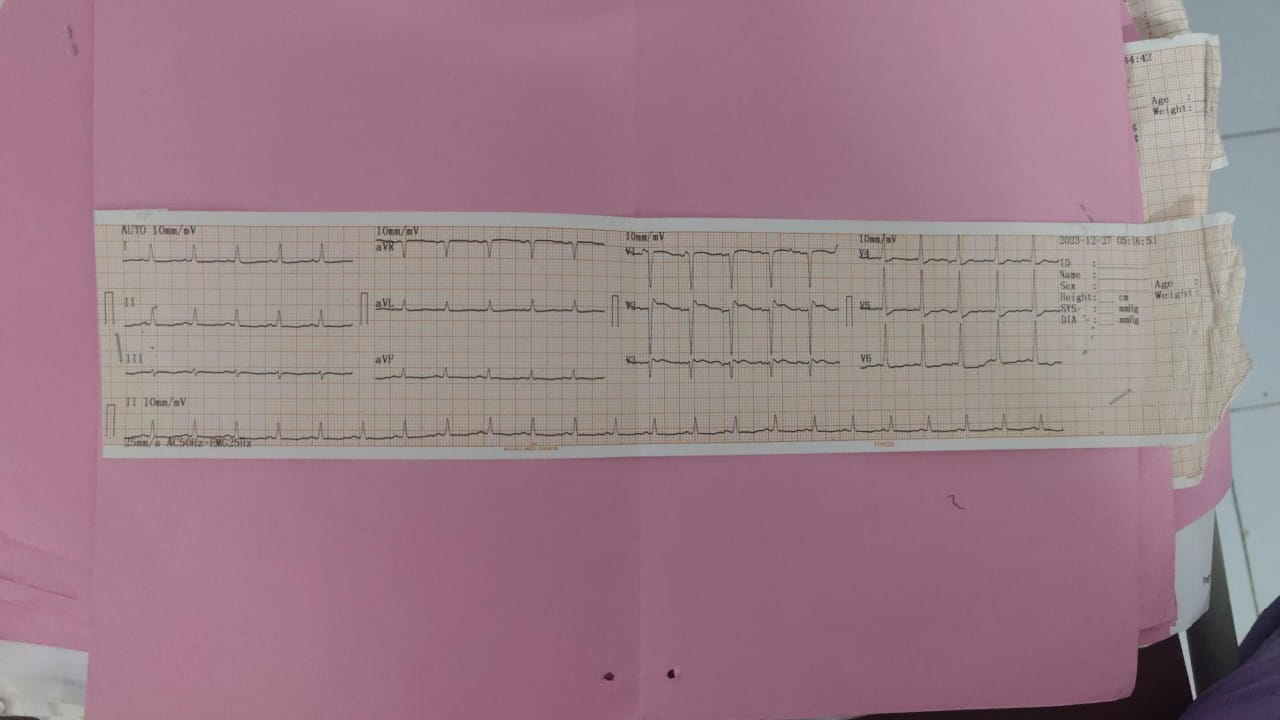
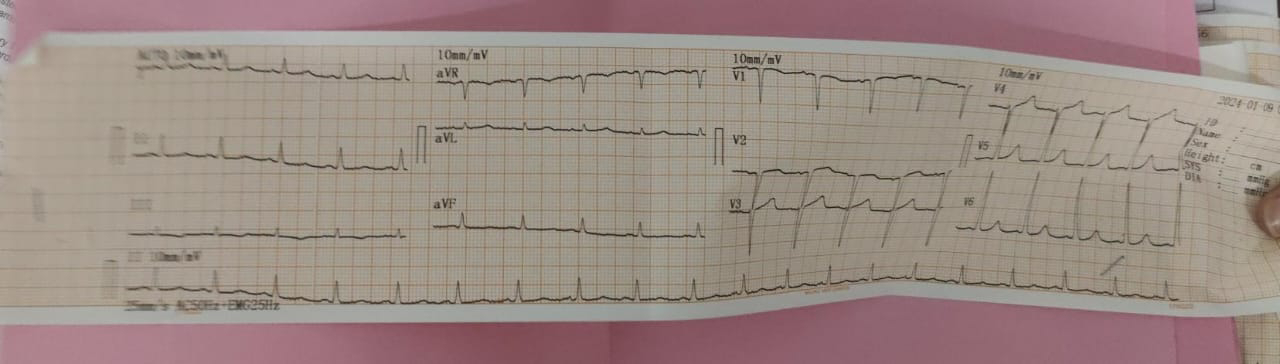
ECG
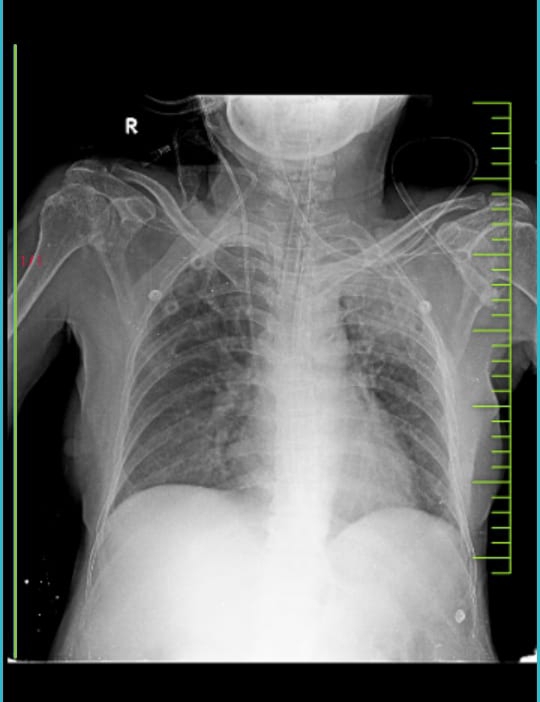
CHEST X RAY
USG ABDOMEN AND PELVIS
2D ECHO
FINAL FIAGNOSIS :
CAD- HEART FAILURE WITH REDUCED EJECTION FRACTION
S/P ON MECHANICAL VENTILATION
CARDIOGENIC SHOCK ? SEPTIC SHOCK
ACUTE PULMONARY EDEMA
SEVERE LV DYSFUNCTION
LEFT UPPER LOBE FUNGAL BALL ?ASPERGILLOMA
DIABETIC KETOACIDOSIS
DIABETIC FOOT ULCER
PSVT- SR
GRADE III BEDSORE
TREATMENT :
COURSE IN THE HOSPITAL
DAY 0 ADMISSION
After 4 hours of admission patient had sudden onset bradycardia, hypotension and decreased responsiveness, crash intubation was done in view of low GCS and type II respiratory failure (Ph- 6.95; pco2- 62mmhg, po2- 88 mmhg , HCO3- 13 mol/l). Patient was intubated with 6.5 mm ET tube and the position was confirmed.
Patient was connected to mechanical ventilator ACMV -VC mode , fio2-70%, PEEP- 5 mmhg, RR- 16 /min , VT- 450ml and started on sedatives and paralytics.
Patient had paroxysmal supraventricular tachycardia patient was given adenosine dose and later started on amiodarone infusion.
In view of uncontrolled sugars and ketoacidosis patient was started on insulin infusion.
In view of hypotension - ? Cardiogenic and septic shock patient was initiated on doubtamine , noradrenaline and vasopressin infusions
8 hrs post intubation patient had sudden bradycardia and fall in saturations and CPR was initiated as per the latest ACLS guidelines after 2 cycles of CPR , ROSC was achieved.
DAY 1 - 26/12
Pulmonology opinion was taken in view of left upper lobe fungal ball aspergilloma and advices for ET secretions C&S, AFB, GS, fungal stain, fungal C&S
Right jugular Triple lumen catheterisation was done
General surgery opinion was taken in view of ulcer over the left foot - diagnosed as Healing ulcer over the plantar and dorsal aspect of left foot. Debridement was done and regular ASD dressing of wound was adviced.
Day 2 - 27/12
Day3 -28/12
Day4 -29/12
Day 5 - 30/12
Day6- 31/12
Day 7 -01/01
Day 8 - 02/01
Day 9 -03/01
Day 10 -04/01
Day 11-05/01
Day 12-06/01
Day 13-07/01
Day 14 -08/01
Day 15 - 09/01
Patient was discharged.
Discussion
The reason for selecting this case is a 65 year old female who presented with the ACS with PSVT and heart failure with reduced ejection traction, who was on mechanical ventilation for six days and has successfully come out of ventilator to lead a normal life
The patient has admitted with us, 10 days back period during which her during his her cardiac activity was completely normal which was shown in the 2d echo, But within a span of 10 days, what has led to her drastic change in her cardiac status?
The patient presented to us in a diabetic ketoacidosis state with uncontrolled sugars was this the acute cause for the development of MI.
Which was the most important factor for the development or the complete recovery of her cardiac failure?
At admission patient has severe metabolic and respiratory acidosis with decompensated heart failure.And it had complete recovery.Even after post CPR status of 5 minutes.
What is the role of dobutamine in improving the cardiac contractility in a case of heart failure with reduced ejection fraction?
In anyway is the diabetic foot ulcer or the wound on the foot is responsible for the development of coronary artery disease and heart failure.
The clinical complexity would be an advanced CAD with heart failure with reduced ejection fraction, PSVT, Diabetic ketoacidosis, Diabetic wound ulcer, left upper lobe fungal ball
What would be the relevance of the family stressors and not being taken care of by the other son and being dependent on her daughter for food and shelter would have affected her daily routine and life that is leading to the development of coronary artery disease and heart failure.
This patient is one of the real case OSCE in which patient of elderly age, with coronary artery disease and reduced ejection and with severe metabolic acidosis who was intubated and was successfully extubated after a course of seven days.
Articles
1)
Acute coronary syndrome and diabetic ketoacidosis : the chicken 🐔 or the egg 🥚
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6736820/#:~:text=The%20association%20of%20DKA%20with,mechanisms%20behind%20this%20strong%20relationship.
2)
There are various cardiovascular complications in ketoacidosis secondary to electrolyte disturbances and catecholamine release. Pulmonary edema can also result, and patients with acute myocardial infarction (MI) may be predisposed to ketoacidosis, which in turn further causes damage to the myocardium.11
Ketoacidosis results in electrolyte imbalances, especially reductions in potassium, magnesium, and phosphorus, which can result in cardio-vascular complications if not carefully replaced
https://www.uspharmacist.com/article/cardiovascular-complications-of-ketoacidosis
3)
And in the end I would also like to emphasise on the importance of psychological factors in cardiovascular health. In this case the psychosocial factors of importance were that pt..son…whatever it is tell that .
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3653260/
The technical difficulties
Patients admitted with Diabetic ketoacidosis (DKA) are often volume depleted and require large volumes of intravenous fluids for resuscitation. Large volume resuscitation can have major impacts on the mortality, length of hospital stay in the Heart failure population with reduced ejection fraction. This is another issue in tackling this kind of patients.
You can mention about it but before that search and see if there are any guidelines to treat patients with DKAHF
------
DKA valla oche electrolyte abnormalities (Mg,Po4,K) might have precipitated a PSVT,and PSVT could have triggered the heart failure.In that case the heart failure will recover after controlling the arrhythmia and electrolyte abn
------
So there are 4 possibilities
1.DKA causing heart failure due to acidosis causing myocardial depression
2.DKA,electrolyte abn,PSVT then heart failure
3.MI causing DKA
4.Plus or minus pre existing coronary artery disease that sometimes won’t be evident on echo.